Maybe I’m biased because I’m a woman, but I truly believe there’s a lot to gain from understanding some of the most common health issues affecting women today. If more people took the time to learn about these conditions, I genuinely think the world would be a more compassionate and supportive place. One of the key conditions that deserves more awareness is Endometriosis – a misunderstood and often overlooked disease that causes significant distress for many women.
Endometriosis is an inflammatory disease where tissue similar to the lining of the uterus grows outside of it. This tissue can attach to the ovaries, fallopian tubes, the outer surface of the uterus, and other organs in the pelvis (1, 2, 3). In rare cases, it may even be found outside the pelvic area. This misplaced tissue causes pain and can lead to serious complications, including infertility.
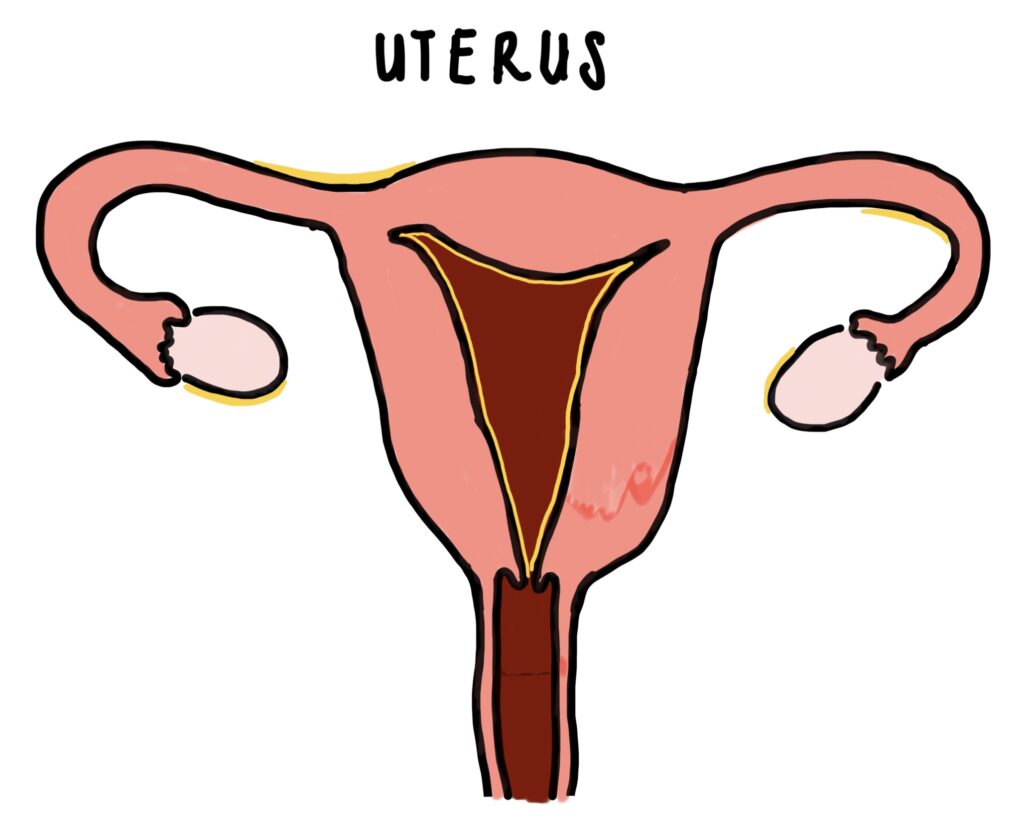
Figure 1 – Illustration of the uterus showing endometriosis tissue in yellow. Created by Dr. Mojibola Orefuja.
Normally, the uterine lining builds up and sheds each month during a woman’s menstrual cycle. With Endometriosis, the tissue outside the uterus behaves similarly – it thickens, breaks down, and bleeds. But because it’s not in the right place, the blood and tissue can’t exit the body properly. This leads to pain, inflammation, and often scarring, which can make symptoms worse over time (2).
Endometriosis is surprisingly common, affecting around 10% of women and girls of reproductive age worldwide. Yet, it often goes undiagnosed for years. Most women are diagnosed between the ages of 18 and 29, meaning many have likely lived with pain long before getting any answers. There also appears to be a genetic link as women with a close relative who has Endometriosis are more likely to develop it themselves.
Causes and Risk Factors
The truth is, we don’t yet know exactly what causes Endometriosis. Several theories have been suggested, but none fully explain the condition. Here are two of the most well-known:
- Retrograde Menstruation – This is when menstrual blood flows backward through the fallopian tubes into the pelvic cavity instead of leaving the body. This blood contains uterine lining cells, which can attach to pelvic organs, grow, and cause problems (2).
- Cell Transformation – Some researchers believe that certain cells in the abdomen (called peritoneal cells) can transform into cells similar to those found in the uterus under the influence of hormones and immune factors (2).
Risk factors for developing Endometriosis include (2):
- Never having given birth
- Starting periods at an early age
- Going through menopause later in life
- Having short menstrual cycles
Signs and Symptoms
The most well-known symptom of Endometriosis is pelvic pain – often severe and sometimes debilitating. This pain can occur:
- During periods (and can be much worse than typical period pain)
- During sex
- While urinating or having a bowel movement
This kind of pain can deeply affect a woman’s quality of life and make it difficult to explain just how bad it really is (1).
Other common symptoms include:
- Heavy or irregular bleeding
- Bloating
- Nausea
- Fatigue
- Difficulty getting pregnant
Because of how long it can take to diagnose and how chronic the condition can be, many women also struggle with mental health issues like anxiety and depression.
Diagnosis and Investigations
Unfortunately, Endometriosis is often hard to diagnose. It can mimic other gynaecological or gastrointestinal conditions like Adenomyosis, Fibroids, Pelvic Inflammatory Disease, and even Irritable Bowel Syndrome. Doctors may begin with:
- A pelvic exam (which may include an internal vaginal examination)
- Blood tests to check for inflammation or other causes
- Ultrasound or MRI scans to visualize internal organs
The gold-standard test for diagnosis is called a diagnostic laparoscopy. This is a minor surgical procedure where a small camera is inserted through tiny incisions in the abdomen to directly look for signs of Endometriosis. If the tissue is found, a biopsy may be taken. However, because this is a surgical procedure with associated risks, it’s not typically the first test doctors will recommend.
Treatments
There’s currently no cure for Endometriosis, but treatments can help manage the symptoms and improve quality of life. Treatment options fall into two main categories:
1. Medications
- Pain relief: Over-the-counter medications like paracetamol or ibuprofen
- Hormonal treatments: Such as the combined oral contraceptive pill (COCP), hormone-releasing implants, or IUDs
2. Surgery
- During a diagnostic laparoscopy, doctors may also perform a procedure called ablation, where the endometriosis tissue is burned away to reduce pain and slow progression.
Endometriosis is a condition that affects millions of women around the world, yet many still suffer in silence or struggle for years without a diagnosis. Raising awareness and understanding is the first step toward better outcomes – for ourselves, our friends, and our communities. If you or someone you know is experiencing symptoms like those described above, don’t hesitate to speak to a healthcare provider. The sooner Endometriosis is identified, the sooner treatment can begin.
Useful links to check out:
- Endometriosis UK – The leading UK charity providing information, support, and advocacy.
- NHS – Endometriosis Overview – Official NHS page with symptoms, diagnosis, and treatment information.
- The British Society for Gynaecological Endoscopy (BSGE) – Includes a list of accredited Endometriosis specialist centres in the UK.
References:
- World Health Organization. Endometriosis [Internet]. 2023 [cited 2025 Jun 9]. Available from: https://www.who.int/news-room/fact-sheets/detail/endometriosis
- Mayo Clinic. Endometriosis: Symptoms and causes [Internet]. 2024 [cited 2025 Jun 9]. Available from: https://www.mayoclinic.org/diseases-conditions/endometriosis/symptoms-causes/syc-20354656
- National Health Service (NHS). Endometriosis [Internet]. 2023 [cited 2025 Jun 9]. Available from: https://www.nhs.uk/conditions/endometriosis/
- Endometriosis UK. Endometriosis UK: Support, information and advocacy [Internet]. 2023 [cited 2025 Jun 9]. Available from: https://www.endometriosis-uk.org/
- BMJ Best Practice. Endometriosis [Internet]. 2024 [cited 2025 Jun 9]. Available from: https://bestpractice.bmj.com/topics/en-gb/355
