When you think of OCD, your mind might jump straight to that friend who’s a bit of a “clean freak” or who loves their routines a little too much. But that’s a really common and unfortunately harmful misconception.
People living with OCD (Obsessive-Compulsive Disorder) struggle far more than most realise. If you have OCD yourself or know someone who does, you’ve probably seen how difficult it can be when others dismiss or misunderstand the condition. While OCD can vary in how it shows up from person to person, it’s crucial that we learn what it really is so we can be more supportive, compassionate, and informed.
What Exactly Is OCD?
OCD, short for Obsessive-Compulsive Disorder, is a neuropsychiatric condition defined by two main features: obsessions and compulsions. Let’s break those down.
- Obsessions are persistent, unwanted thoughts, worries, or urges that cause distress.Example: Constantly thinking your house will burn down and your loved ones will die in the fire.
- Compulsions are repetitive behaviors a person feels driven to perform in order to ease the anxiety caused by those obsessions.Example: Repeatedly checking that the oven is turned off, even when you know it is, to make sure the house doesn’t burn down.
The two feed into each other, creating what’s known as the OCD cycle.
An obsession causes distress, the distress leads to a compulsion, the compulsion brings temporary relief, but soon the obsession returns, and the cycle begins again.
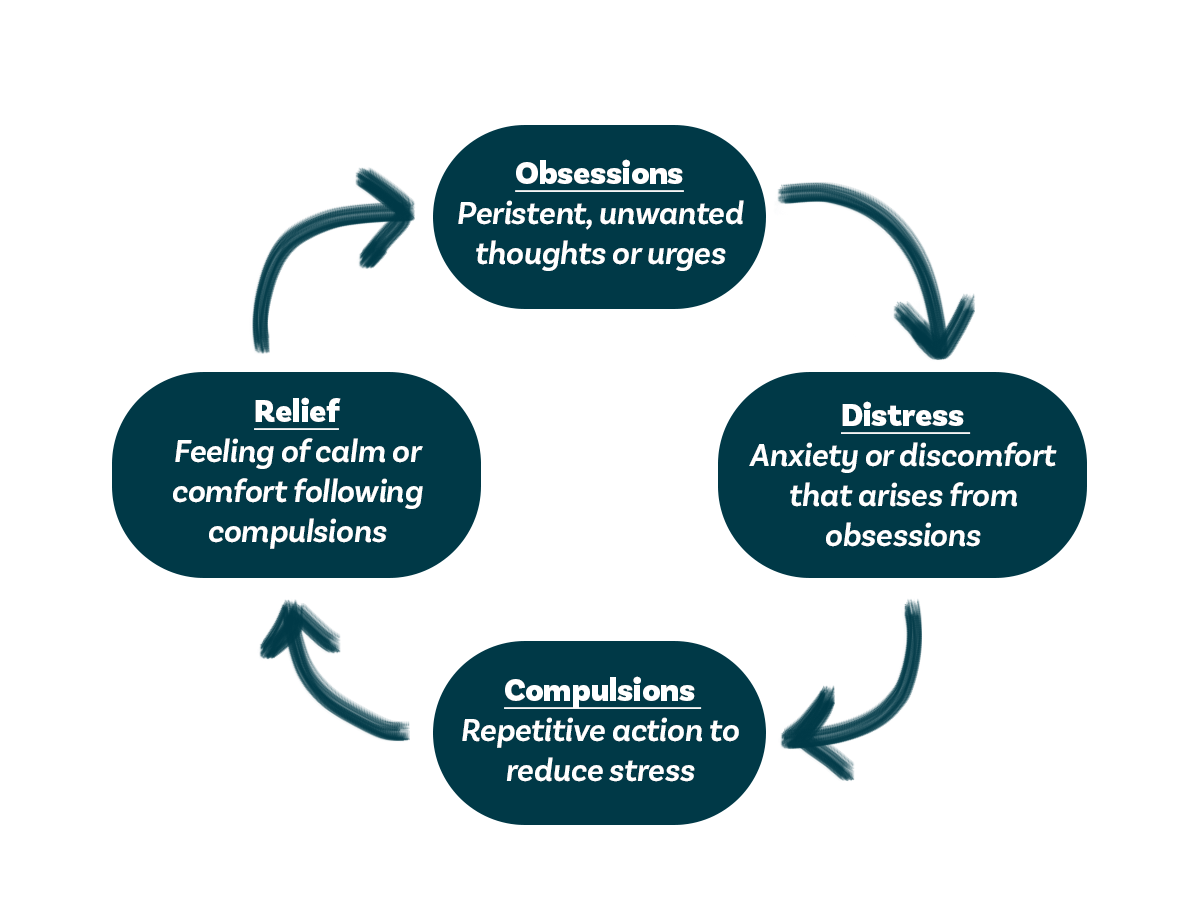
Figure 1 – The OCD Cycle: A visual of how obsessions and compulsions reinforce each other.
What makes OCD so distressing is that these thoughts and behaviours can take up hours of a person’s day, making it hard to focus on work, relationships, or everyday life. Many people with OCD know that their fears or habits don’t make logical sense, but that doesn’t make them any easier to stop.
What Causes OCD?
There isn’t one single cause of OCD. Instead, it develops through a mix of genetic, environmental, and neurological ****factors.
- Genetics: Research, including twin studies, shows that OCD can run in families, suggesting a significant hereditary component (3,4).
- Life experiences: Stressful or traumatic experiences, especially during childhood, can contribute to the onset of OCD. For some, this leads to PTSD; for others, it manifests as OCD.
- Brain function: Studies also show that certain brain circuits involved in regulating behaviour and outcomes can become dysregulated in people with OCD, leading to intrusive thoughts and repetitive actions.
Since OCD often appears alongside other mental health conditions, such as anxiety or depression, it’s believed that a combination of these factors contributes to its development.
Common Symptoms of OCD
We’ve already mentioned obsessions and compulsions, but let’s look at how these might appear in real life.
Obsessions are intrusive, repetitive, and often irrational thoughts that cause intense anxiety or shame. People with OCD may feel too embarrassed to share them, fearing judgment or misunderstanding.
Common obsessions include (1):
- Fear of contamination by people or the environment. This is much more than disliking dirt; it’s an overwhelming fear of germs or disease.
- Fear of harming others or being harmed.
- Worry that something is incomplete or “not quite right.”
- An intense need for order, symmetry, or exactness.
Compulsions are repetitive or ritualistic actions used to temporarily relieve the anxiety caused by obsessions (1):
- Excessive hand-washing or showering.
- Repeated cleaning of already clean items.
- Rearranging or ordering things until they feel “just right.”
- Checking locks, appliances, or switches over and over.
For some people, these behaviours can become dangerous or all-consuming, so it is important that they seek help.
How OCD Is Treated
Treating OCD often takes a biopsychosocial approach, meaning therapy targets the biological, psychological, and social aspects of the condition.
1. Biological
- Medication: Selective Serotonin Reuptake Inhibitors (SSRIs) are often prescribed and have been shown to be effective in managing OCD symptoms.
- Neuromodulation therapy: A type of brain stimulation that uses magnetic fields, and is well tolerated by most individuals.
2. Psychological
- Cognitive Behavioral Therapy (CBT): This is the first-line treatment for OCD, particularly Exposure and Response Prevention (ERP) therapy. It helps individuals face their fears and resist the urge to perform compulsions, gradually reducing their intensity and frequency.
3. Social
Encouraging open communication is key. Talking about obsessions with trusted family members or therapists helps break the shame and isolation OCD can cause. Confronting these fears in a supportive environment is often a crucial step toward recovery.
OCD is often misunderstood, but it is a very real and often debilitating mental health condition. The good news is that with the right support and treatment, people living with OCD can absolutely lead fulfilling, balanced lives. The next time you hear someone joke about being “so OCD,” take a moment to remember what this disorder truly means. Understanding and compassion go a lot further than stereotypes ever will.
