Happy Monday! I’m back this week with a new blog post that links to our last entry on Hypertension. Yes, we’ve all seen the adverts and posters, but many people still choose to prioritise comfort over health. I know it feels nice to eat whatever you want, avoid exercise, or engage in risky health behaviours like excessive smoking and drinking, but these habits have a huge effect on your heart health, and heart health is essential if you want to live a long, happy life.
Over the next few blog entries, my aim is to encourage you and show you why healthy living truly benefits you. With this in mind, today’s post focuses on Acute Coronary Syndrome (ACS), which is the name for a range of heart disorders that occur when the coronary arteries become dangerously narrowed or blocked (1), including heart attacks. ACS affects roughly 93,500 individuals in the UK every year (2), and studies also show that men are twice as likely to suffer from ACS compared to women. There are many risk factors that contribute to the development of ACS.
Causes of ACS
Like any organ in the body, the heart has its own blood supply, which allows it to receive enough oxygen to keep pumping blood to the rest of the body. These blood vessels are known as the coronary arteries. When the arteries become increasingly narrow and eventually blocked, the heart muscle becomes damaged. This occurs because the muscle receives less oxygen, causing the affected tissue to break down and die.
We classify the different types of ACS based on the degree of damage caused to the heart muscle, measured using clinical tests. Different levels of artery narrowing result in different levels of muscle damage, which can be seen in Figure 1. In Part 1 of the diagram, the artery is only partially blocked, causing a small amount of damage. In Part 2, the artery is completely blocked, resulting in much more extensive damage, shown by the wider brown area on the heart muscle.
Two keywords that help describe the degree of damage seen in heart disease are:
- Ischaemia – reduced blood supply to an organ
- Infarction – complete blockage of blood supply to an organ, leading to tissue death. This is usually caused by a blood clot blocking an artery or by part of a clot obstructing smaller blood vessels.
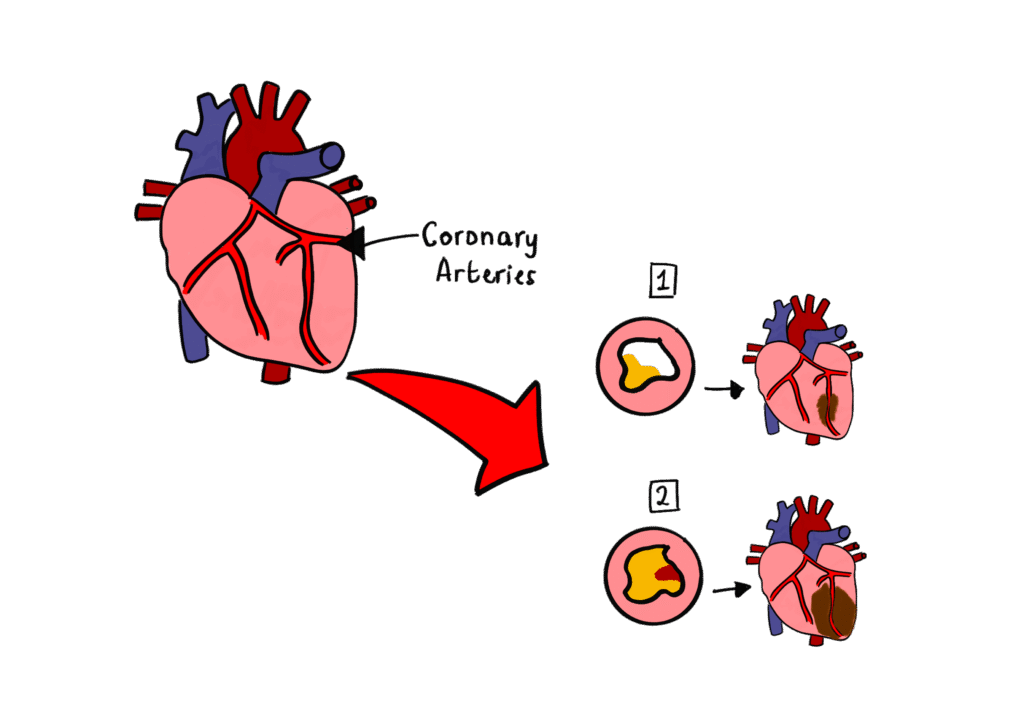
Figure 1: Diagram of the Heart and Coronary Arteries – This figure shows the difference in damage to the heart when the coronary arteries are obstructed. The brown shaded areas represent muscle death. Created by Dr Mojibola Orefuja.
The journey to heart disease caused by narrow and blocked arteries depends on multiple risk factors. Diet plays a major role, especially the types of food we eat. Foods high in fat and cholesterol are harmful when consumed in large amounts because they form deposits within the artery walls. In Figure 1, the yellow build-up represents these fatty and cholesterol deposits. When this build-up becomes severe, it can rupture and cause a blockage.
Other contributing factors include lack of exercise and excessive smoking:
- Lack of exercise – Exercise helps maintain good heart function by enabling the heart muscle to pump efficiently. Without exercise, the heart has to work harder to supply the body with oxygen, increasing strain on the heart.
- Excessive smoking – Tobacco smoke contains harmful chemicals that damage the lining of blood vessels, making arteries more prone to fatty build-up and injury from high blood pressure, a major risk factor for heart attack.
Other risk factors include high blood pressure, discussed in detail in the previous post, and a strong family history.
Types of ACS and Its Tests
Acute Coronary Syndrome has three main types: Unstable Angina, Non-ST Elevated MI, and ST-Elevated MI. These medical terms are based on clinical test results. When someone arrives at hospital with symptoms such as chest pain or shortness of breath, two main tests are performed:
- Troponin Blood Test – When heart muscle cells die, they release troponin into the bloodstream. Higher troponin levels indicate more damage.
- Electrocardiogram (ECG or EKG) – This test assesses the electrical signals in the heart and helps identify which area has been affected.
Using these tests, we can identify the type of ACS:
Unstable Angina – Not classified as a heart attack because there is no heart muscle damage. Patients have normal troponin levels and no ECG changes, though their chest pain resembles that of a heart attack and does not improve with rest.
Non-ST Elevated Myocardial Infarction (NSTEMI) – A type of heart attack with raised troponin levels but less dramatic ECG changes. The pain can still be severe.
ST-Elevated Myocardial Infarction (STEMI) – The most serious form, with high troponin levels and clear ECG changes. Immediate treatment is essential to prevent sudden death as heart muscle continues to die.
Signs and Symptoms
Symptoms of ACS include:
- Sudden, intense chest pain
- Pain spreading to the jaw, neck, or shoulders (especially the left side)
- Chest tightness
- Shortness of breath
- Dizziness
- Nausea
- Sweating
This list is not exhaustive, but these symptoms are major warning signs, especially when they occur suddenly.
Treatments
Treatment varies depending on severity and test results.
Medication treatment includes:
- Morphine – this is a strong painkiller which helps with managing the chest pain that comes with ACS
- Oxygen therapy – this is used in patients with STEMI mostly, because patients experience the most pain due to reduced oxygen supply to the heart muscle. By increasing the amount of oxygen in the blood, we can also increase the amount of oxygen getting to these areas that have limited supply.
- Strong doses of blood thinners like Aspirin and Clopidogrel, which help to reduce the chances of an artery getting more blocked.
- Medicines that open up the arteries even more called vasodilators, like nitrates
Interventional Management of ACS
Severe cases require procedures such as Percutaneous Coronary Intervention (PCI), where cardiologists open the blocked artery and keep it open using guided imaging. Not all patients require PCI; only those with confirmed or high-risk blockages.
Secondary Prevention
This step aims to prevent future episodes. Once someone has had a heart attack, their risk of another increases significantly. Long-term blood thinners, blood pressure medications, and lifestyle changes are essential to reduce this risk.
Acute Coronary Syndrome is a serious and often life-threatening condition, but understanding how it develops and how it is treated can empower you to take control of your heart health. Many of the risk factors, such as diet, exercise, and smoking, are within our control, which means we all have the ability to reduce our chances of developing ACS. Small, consistent changes in lifestyle can make a huge difference. My hope is that this post encourages you to prioritise your heart, make healthier choices, and recognise the importance of early action when symptoms arise. Your heart works tirelessly for you, so take care of it in return.
