Sickle Cell Disease, Sickle Cell Anaemia, Sickle Cell Trait. These are all terms we have heard used quite loosely when thinking about Sickle Cell Disease (SCD), but what do each of these terms mean, and how do they affect us? As a black woman, SCD is a disease that is very important to me. Black people are predominantly affected by this disease (1) and as a result of this, it is very important that more of us understand just how much it can affect our lives and the lives of those we love.
All above statistics can be found from source 4.
Causes
SCD happens when someone’s red blood cells take on an unusual crescent or sickle shape – hence the name. Think of it as a building block issue: everyone gets genes from both parents, and these genes tell the body how to make important proteins, especially hemoglobin in blood cells (2,3).
In healthy blood, haemoglobin helps create round, donut-shaped cells that flow smoothly through blood vessels. But when someone has SCD, they inherit two faulty genes – one from each parent – leading to misshapen blood cells. These sickle-shaped cells can stick together and block blood vessels, causing what doctors call a “vaso-occlusive event“. This can lead to a sickle cell crisis (2,3).
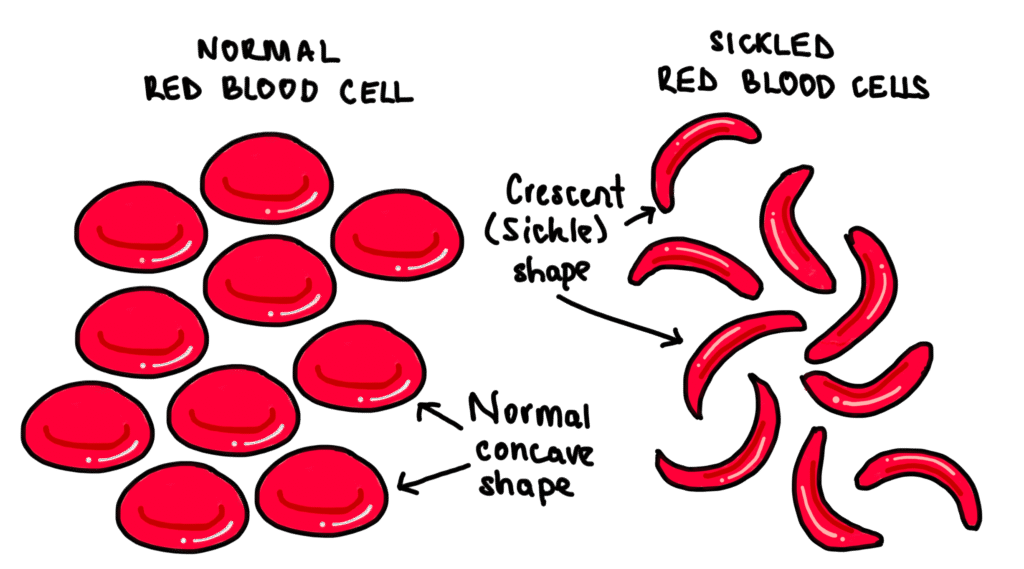
Image created by Dr Mojibola Orefuja
Let’s break down how SCD genes work. A person can only have SCD if they inherit one faulty gene from both mum and dad. The genetic combinations are written like this:
- AA – normal genes, no sickle cell trait
- AS – one normal gene, one faulty gene (this person is a carrier)
- SS – two faulty genes (this person has sickle cell disease)
Here’s what happens with different parent combinations:
- When both parents have normal genes (AA): Their children will always have normal hemoglobin and healthy red blood cells. No carriers, no disease.
- When both parents are carriers (AS): There’s a mix of possibilities:
- 25% chance of a child with normal genes (AA)
- 50% chance of a carrier child (AS)
- 25% chance of a child with SCD (SS)
- When both parents have SCD (SS): All their children will have SCD.
- When one parent has normal genes (AA) and one is a carrier (AS): Their children will either have normal genes or be carriers. None will have SCD.
- When one parent is a carrier (AS) and one has SCD (SS): Their children will either be carriers or have SCD.
- When one parent has normal genes (AA) and one has SCD (SS): All their children will be carriers.
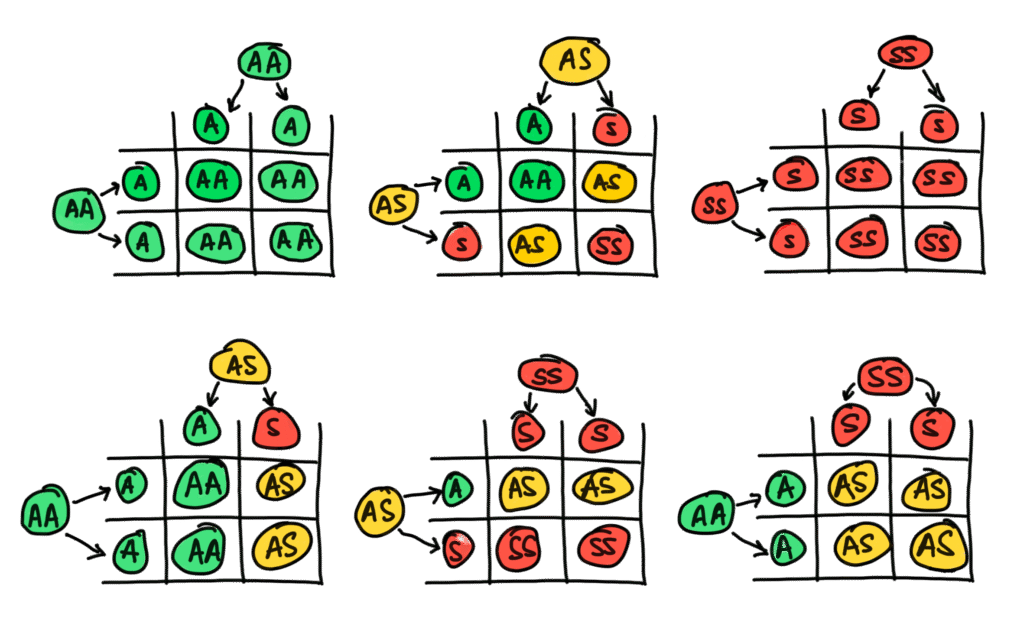
Image created by Dr Mojibola Orefuja
Signs and Symptoms
SCD usually shows its first signs in early childhood (5, 6, 10). Here are the most common symptoms:
- Painful episodes called Sickle Cell Crises – these can be intense and last from days to weeks
- Frequent infections
- Anaemia, which brings along:
- Pale skin
- Shortness of breath
- Dizziness
- Extreme tiredness
People might also experience:
- Slower growth during childhood and delayed puberty
- Stomach pain and yellowing of the skin (jaundice)
- Pain in bones and joints
- Wounds on the legs that take time to heal
Screening for SCD (Diagnosis)
In England, healthcare providers take SCD seriously – so seriously that it’s part of routine screening. Testing can happen during pregnancy or right after a baby is born, and it’s as simple as a blood test. Because symptoms start showing up in childhood, most people with SCD get diagnosed early. It’s pretty rare for someone to reach adulthood without knowing they have it.
Common Organ Complications
Let’s break down some of the main health challenges people with SCD face:
Ongoing Anaemia – This is a constant companion for people with SCD. Because their red blood cells aren’t the right shape, they can’t carry enough hemoglobin in their blood. This causes some of the symptoms mentioned above like pale skin, breathing problems and fainting (10).
Transient Red Cell Aplasia – Sometimes, usually after a viral illness, the body can temporarily stop making red blood cells. This is a complex complication to understand, but it is treatable (10).
Acute Chest Syndrome – Think of this as a lung emergency. It happens when those sickle-shaped cells clump together in lung blood vessels, causing swelling and irritation (11).
Spleen Problems (Splenic Sequestration) – When sickled cells clog up blood vessels in the spleen, it can swell and become painful. This isn’t just uncomfortable – it can cause hemoglobin levels to drop dramatically, leading to breathing problems, fainting, and extreme tiredness (8).
Gallstones – People with SCD are more likely to develop gallstones because their red blood cells break down faster than usual. All that extra breakdown material can form stones in the gallbladder (9).
Infections – Fighting off infections is harder for people with SCD, especially children whose immune systems are still developing. Any sign of infection gets taken very seriously – doctors often start antibiotics right away because sepsis (a dangerous infection response) is a real concern.
Treatment
Managing a Sickle Cell Crisis
Living with SCD is different from dealing with many other conditions. Instead of having constant symptoms, people experience periods of crisis followed by times of stability. During these crisis periods, two main issues usually need immediate attention: pain and fever.
Dealing with Pain
- Sometimes regular painkillers or even mild opioids like Codeine aren’t enough during severe crises
- Healthcare providers aim to offer pain relief within 30 minutes when someone arrives at the emergency department
Managing Fever
- For anyone with SCD who has a temperature above 38.5°C (or 38°C in kids under 12), broad-spectrum antibiotics are usually given right away
- This quick action is necessary because infections can be dangerous for people with SCD
Other crisis symptoms that need attention include:
- Dehydration (from vomiting or diarrhea)
- Extreme paleness or jaundice
- Blood in the urine
If you have SCD and you ever experience these symptoms, please seek medical attention immediately.
Long-term Care
Managing SCD for the long haul takes a team effort. While specialists play important roles, much of the care happens at the local level with GPs and community healthcare teams.
There are some treatment options that are good to know about when it comes to SCD. These are:
Hydroxyurea: This medication helps reduce the frequency of painful episodes. Studies show it’s beneficial because it (7):
- Cuts down on how often painful crises occur
- Reduces organ damage in children (protecting kidneys, spleen, brain, and other organs)
- Helps promote proper growth and development
Blood Transfusions: Regular blood transfusions are crucial for both children and adults with SCD. While they effectively address most symptoms, they’re usually part of a broader treatment plan. Doctors still need to find and treat what triggered the crisis to prevent things from getting worse.
Understanding SCD – from how it’s inherited to how it affects daily life – helps us support those living with the condition and their families. While the number of people affected by SCD continues to grow globally, advances in treatment and care mean better outcomes for patients. For anyone concerned about SCD, especially those planning to have children, speaking with healthcare providers about genetic testing and management options is an important first step. The more our community understands about SCD, the better we can support those affected by it.
References:
- National Institute for Health and Care Excellence (NICE). Prevalence | Background information | Sickle cell disease | CKS | NICE [Internet]. Available from: https://cks.nice.org.uk/topics/sickle-cell-disease/background-information/prevalence/
- National Health Service (NHS). Sickle cell disease – NHS [Internet]. Available from: https://www.nhs.uk/conditions/sickle-cell-disease/
- Sickle Cell Society. About Sickle Cell [Internet]. Available from: https://www.sicklecellsociety.org/about-sickle-cell/#:~:text=3 Approximately 1 in 79,with sickle cell each year.
- GBD 2021 Sickle Cell Disease Collaborators. Global, regional, and national prevalence and mortality burden of sickle cell disease, 2000–2021: a systematic analysis from the Global Burden of Disease Study 2021. *Lancet Haematol.*2023;10:e585–99. Available from: https://doi.org/10.1016/S2352-3026(23)00118-7
- National Perinatal Epidemiology Unit (NPEU). Sickle Cell Disease | UKOSS [Internet]. Available from: https://www.npeu.ox.ac.uk/ukoss/completed-surveillance/scd
- National Institute for Health and Care Excellence (NICE). Sickle cell disease | Management | CKS | NICE [Internet]. Available from: https://cks.nice.org.uk/topics/sickle-cell-disease/management/
- Agrawal RK, Patel RK, Shah V, Nainiwal L, Trivedi B. Hydroxyurea in sickle cell disease: drug review. Indian J Hematol Blood Transfus. 2014;30(2):91–6. Available from: https://doi.org/10.1007/s12288-013-0261-4
- Kane I, Kumar A, Atalla E, et al. Splenic sequestration crisis [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 [updated 2023 Jun 5; cited 2025 Jan]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK553164/
- Alder Hey Children’s NHS Foundation Trust. Sickle Cell Disease Chronic Complications: Gallstones [Internet]. Available from: https://www.alderhey.nhs.uk/conditions/patient-information-leaflets/sickle-cell-disease-chronic-complications-gallstones/#:~:text=Gallstones are hard%2C pebble like,Clay-coloured stool
- BMJ Best Practice. Sickle Cell Disease: Complications [Internet]. Available from: https://bestpractice.bmj.com/topics/en-gb/100/complicationsSickle cell anaemia.pdf
- American Lung Association. Acute Chest Syndrome (ACS) [Internet]. Available from: https://www.lung.org/lung-health-diseases/lung-disease-lookup/acute-chest-syndrome#:~:text=Acute chest syndrome (ACS) is,Read More
- Imperial College Healthcare NHS Trust. Gene editing for sickle cell approved for use on the NHS [Internet]. Imperial College Healthcare NHS Trust; 2025 Feb 4 [cited 2025 Feb 4]. Available from: https://www.imperial.nhs.uk/about-us/news/gene-editing-for-sickle-cell-approved-for-use-on-the-nhs

medicinal plant like zanthoxylum zanthoxyloides that grows naturally in certain parts of Africa has been applied as palliative for sickle cell disease.
As a sickle cell warrior i have observed that in Midlands hospitals some doctors and nurses are still not knowledgable what sickle cell disease is.I have come across some of them asking when did it start or how i get it.
I can’t see it taken seriously as we still have to wait hours at emergency when in crisis
I am so sorry you have had to experience this.
This is exactly why I wrote the post though, many healthcare providers in this country still don’t fully understand Sickle Cell Disease. Unfortunately, it is our responsibility to make sure we educate them every chance we get.