Pause for a moment. Think about the people you know who may have PCOS. Now, consider how much you actually understand about what they’re going through. PCOS (polycystic ovary syndrome) is more common than you might think, affecting many women, often from a young age, yet society doesn’t talk enough about how difficult it can be to live with. Like many health conditions that mainly affect women, PCOS can feel overwhelming, and for those diagnosed, it can sometimes seem like a life sentence with no clear solution in sight. I’m not here to pretend I know everything there is to know about PCOS, but I do want to help you understand it a bit better. If your mother, sister, cousin, or friend has PCOS, this might give you a little more insight into what they’re experiencing.
PCOS is a hormonal condition that affects women of reproductive age—that is, women who get periods. It typically begins in the teenage years and can cause symptoms that fluctuate throughout a person’s life. Unfortunately, PCOS can’t be cured. It’s also surprisingly common, affecting 6-13% of women of childbearing age worldwide (1). Even more surprising? Up to 70% of women with PCOS are undiagnosed (1). PCOS affects both the body and the mind. Physically, it can cause hormonal imbalances that disrupt the reproductive system and make it harder to get pregnant. In fact, PCOS is one of the leading causes of infertility in women.
Whats Happening in the Body?
So, what’s actually going on inside the body of someone with PCOS? Simply put, the condition is linked to having polycystic ovaries. Let’s break it down.
Normally, during a woman’s monthly cycle, one dominant follicle develops inside the ovaries. This follicle releases an egg during ovulation (2). But in women with PCOS, multiple follicles develop without releasing eggs (2,3). Take a lok at the diagram below (Figure1). These underdeveloped follicles can form small cysts in the ovaries, which is where the term “polycystic” comes from. This failure to ovulate is a key reason why women with PCOS often struggle with infertility.
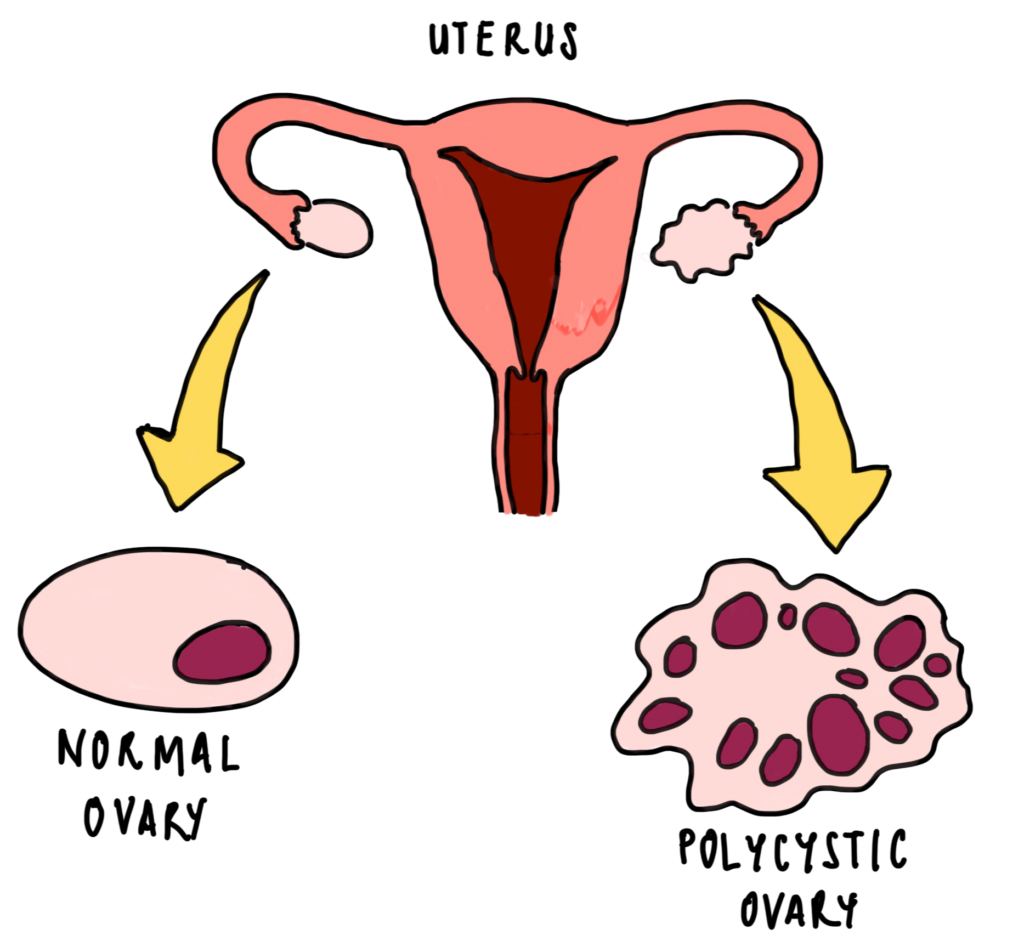
Figure 1 – Image created by Dr Mojibola Orefuja from Source 2.
But there’s more. When eggs aren’t released, the ovaries produce more hormones called androgens (4). Androgens, including testosterone, are typically produced in small amounts in women. However, in women with PCOS, these levels are higher than normal, which leads to some of the classic PCOS symptoms, such as excess body hair and acne.
Another hormone involved is insulin, which helps regulate blood sugar. Many women with PCOS have insulin resistance, meaning their bodies don’t respond properly to insulin. This causes blood sugar levels to rise, prompting the body to produce even more insulin. Elevated insulin levels can worsen PCOS symptoms and contribute to weight gain and hormonal imbalances.
To sum up, three key hormonal issues are at play in PCOS:
- A build-up of underdeveloped follicles (cysts) in the ovaries
- Excess androgen production
- Insulin resistance and high insulin levels
Risk Factors
The exact cause of PCOS is still unclear, but genetics likely play a role. If your mother or sister has PCOS, you may be at higher risk. Researchers believe certain genes may make some people more susceptible to developing the condition.
Signs and Symptoms
Recognizing the symptoms of PCOS is crucial because early diagnosis can make a big difference. Hormonal imbalances in PCOS can cause a range of symptoms, including (2):
- Irregular periods or no periods at all
- Excess facial or body hair (known as hirsutism)
- Thinning hair or male-pattern baldness
- Weight gain or difficulty losing weight
- Oily skin and acne
- Reduced fertility or infertility
Another lesser-known symptom is darkened patches of skin, often found in skin folds like the armpits, neck creases, and under the breasts.
Living with these symptoms can be physically and emotionally exhausting. Many women with PCOS also struggle with mental health challenges, including anxiety and depression.
Diagnosis
If you think you might have PCOS, the first step is to talk to your doctor. They’ll start by asking about your symptoms and medical history. This is usually followed by a physical exam, which may include a pelvic exam to check the health of your reproductive organs.
If PCOS is suspected, you may be referred for further tests, such as:
- Ultrasound: A painless scan that uses sound waves to create images of your ovaries. This helps doctors check for multiple ovarian cysts.
- Blood Tests: These tests measure hormone levels, including testosterone, estrogen, insulin, and glucose. Your doctor may also check your cholesterol and lipid levels, as these can be affected by PCOS.
Treatment Options
There’s no one-size-fits-all treatment for PCOS, but managing the condition often involves a combination of lifestyle changes, medications, and symptom-specific treatments (5).
1. Education and Lifestyle Changes
Understanding PCOS is the first step in managing it. Learning about the hormonal imbalances that cause symptoms can help you take charge of your health.
Since PCOS can increase the risk of complications like type 2 diabetes and heart disease (6), adopting healthy lifestyle habits is essential. This includes:
- Regular exercise
- Healthy eating
- Managing alcohol intake
- Prioritizing good sleep
2. Managing Symptoms
Treatment plans are often tailored to address each person’s specific symptoms. Some common approaches include:
- Reducing Androgens: The combined oral contraceptive pill is often prescribed to lower androgen levels. This can also help regulate periods and improve fertility (7).
- Managing Infertility: Women struggling with infertility may be referred to a fertility specialist for further evaluation and treatment.
- Treating Acne: Topical creams and medications can help manage acne, similar to treatments used in people without PCOS.
- Addressing Hair Growth: Unfortunately, there’s no quick fix for excess hair growth. Reducing androgen levels can help over time, but in the meantime, hair removal options can provide some relief.
3. Medications
Metformin, a medication commonly used for type 2 diabetes, may also be recommended for some women with PCOS. It can help improve insulin sensitivity and regulate blood sugar, though its benefits in PCOS are still being studied.
PCOS is a complex condition, and managing it can be challenging. But with the right support, knowledge, and treatment, many women with PCOS go on to live healthy, fulfilling lives. If you think you might have PCOS, don’t hesitate to reach out to your doctor. Early diagnosis and management can make a world of difference. And remember, you’re not alone. There’s a community of women who understand what you’re going through and resources available to help you navigate the journey ahead.
References
- World Health Organization. Polycystic ovary syndrome [Internet]. Geneva: WHO; 2022 [cited 2025 Mar 24]. Available from: https://www.who.int/news-room/fact-sheets/detail/polycystic-ovary-syndrome
- Royal College of Obstetricians and Gynaecologists. Polycystic ovary syndrome (PCOS): What it means for your long-term health [Internet]. London: RCOG; 2023 [cited 2025 Mar 24]. Available from: https://www.rcog.org.uk/for-the-public/browse-our-patient-information/polycystic-ovary-syndrome-pcos-what-it-means-for-your-long-term-health/
- NHS. Polycystic ovary syndrome (PCOS) [Internet]. London: NHS; 2022 [cited 2025 Mar 24]. Available from: https://www.nhs.uk/conditions/polycystic-ovary-syndrome-pcos/
- Johns Hopkins Medicine. Polycystic ovary syndrome (PCOS) [Internet]. Baltimore: Johns Hopkins Medicine; 2021 [cited 2025 Mar 24]. Available from: https://www.hopkinsmedicine.org/health/conditions-and-diseases/polycystic-ovary-syndrome-pcos
- National Institute for Health and Care Excellence (NICE). Polycystic ovary syndrome: Management – adults [Internet]. London: NICE; 2023 [cited 2025 Mar 24]. Available from: https://cks.nice.org.uk/topics/polycystic-ovary-syndrome/management/management-adults/
- National Institute for Health and Care Excellence (NICE). Polycystic ovary syndrome: Complications – background information [Internet]. London: NICE; 2023 [cited 2025 Mar 24]. Available from: https://cks.nice.org.uk/topics/polycystic-ovary-syndrome/background-information/complications/
- Legro RS, Arslanian SA, Ehrmann DA, Hoeger KM, Murad MH, Pasquali R, et al. Combined oral contraceptives in the treatment of polycystic ovary syndrome [Internet]. PubMed; 2005 [cited 2025 Mar 24]. Available from: https://pubmed.ncbi.nlm.nih.gov/15790599/#:~:text=Combined oral contraceptives (COC) are,symptoms and improving menstrual dysfunction
